Clients at The Child Center Residential Treatment Facility, one of many Child Center programs that serve adolescents with mental health needs
The changing face of challenge in American adolescence—and how to meet it
By Jennifer Blitzer, LCSW-R
Program Director, Woodside Youth Intensive Outpatient Program
American adolescence is changing. Three decades ago, the biggest public health threats to teenagers came from binge drinking, drunk driving, teenage pregnancy, and smoking. All have fallen sharply in the United States. In their place are soaring rates of mental illness.
The decline in mental health among teenagers intensified during the COVID-19 pandemic but clearly predates it. In 2019, 13 percent of teenagers reported having a major depressive episode, a 60 percent increase from 2007. Emergency room visits by children and adolescents for anxiety, mood disorders, and self-harm in that period also rose sharply. And for people ages 10 to 24, suicide rates, stable from 2000 to 2007, leaped nearly 60 percent by 2018, according to the Centers for Disease Control and Prevention. Mental illness has soared in all racial groups, socioeconomic statuses, and areas of the country. Urban and rural communities are equally affected.
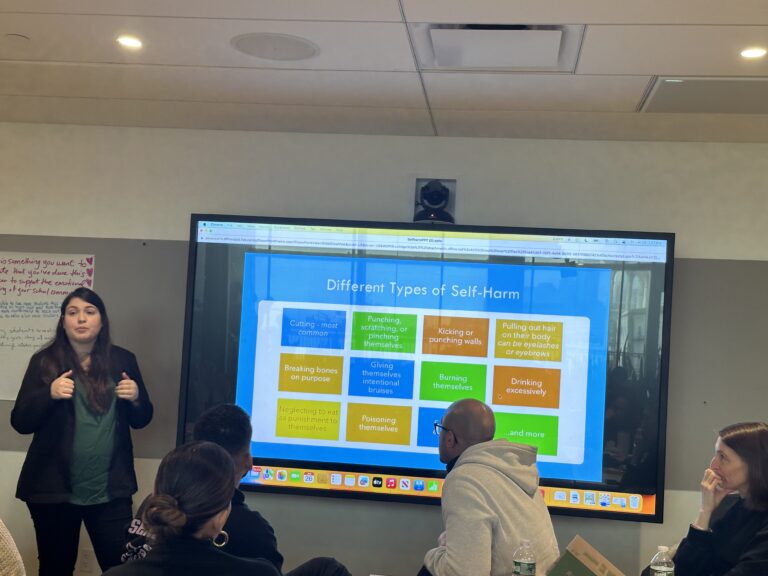
As a clinical social worker for high-risk teens at The Child Center of NY, I have seen these troubling increases firsthand. The Child Center has experienced a surge in referrals from schools, parents, and hospitals seeking help for teenagers who are experiencing severe depression, suicidal behaviors, self-harm, and anxiety.
While the picture seems bleak, it is not without hope. We have a robust body of research that bears out best practices for guiding young people through the very real challenges they face. We know the key is a holistic approach that considers the whole person, engages the whole family, and takes a person-centered, culturally responsive approach that focuses on individual goals and strengths.
Our challenge is to scale up this kind of work and reach as many young people who need our help as possible. This is especially important in immigrant communities, communities of color, and other under-served communities where services are scarce and the stigma against receiving mental health services may be strong.
To help meet this urgent need, The Child Center launched the Youth Intensive Outpatient Program (IOP) at our Woodside Family Wellness Center. Located in the heart of a community with a large immigrant population and high rates of poverty, the IOP was specifically created to serve hard-to-reach populations and treat adolescents who are experiencing mood disorders, suicidal ideation, and severe depression. It’s a short-term, intensive program for adolescents ages 12-17 who present with serious emotional disturbance and are at high risk of self-harm and suicidal behaviors. The program also works to prevent hospitalization for adolescents who need a higher level of care than the weekly-session outpatient settings. Our clinicians use evidenced-based treatment models such as cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT), and the Safety Alternatives for Teens and Youth Program (SAFETY) developed by UCLA.

Blog author Jennifer Blitzer, right, with Woodside IOP Educational Coordinator Arely Hernandez, left
Most important, we take a holistic approach: Because both experience and research tell us that parents and families play a big role in helping teens heal, a parent training model is integral. Because research and experience (and common sense) tell us that people need to know they are more than their diagnosis, we provide educational and vocational support to help clients envision and plan for a bright future based on their individual strengths. And because understanding cultural differences matters, our team members largely come from the community they serve and speak the same language as their clients—literally and figuratively.
Being a clinical social worker for high-risk teens at The Child Center is challenging to say the least, but I couldn’t imagine a better return on investment. Seeing a teen move from despair to hope, witnessing teens and their parents improve their relationships, and having a teen envision a positive future makes me feel motivated and passionate about the work we do at The Child Center. We see real results every day. We recently had a client who had stopped attending school and was actively suicidal—to the point that she had tried running into traffic. After attending sessions in the IOP and having home-based services, the client has no longer been actively suicidal, was less depressed, and had begun the difficult process of addressing her childhood trauma and improving her relationship with her parents. She has a goal to become a doctor or nurse, and she is beginning to pursue that goal by enrolling in SAT prep and extra tutoring so that she has a better chance of being admitted to a top college. She now has a hope and excitement for the future that was unthinkable when she began therapy.
Every one of us can make a difference. If you are a parent, you can make a difference by being alert to key indicators of changes in your child’s behavior: poor sleeping habits, disinterest in previously enjoyed activities, or a decline in academic performance. If you notice your teen has prolonged feelings of sadness and hopelessness, it may be time for professional help. Don’t be afraid to be clear and direct with your teen regarding your concern about their emotional well-being, but do so with compassion and understanding. Many teens have verbalized that they feel like they are being “blamed” for being depressed when spoken to by their parents, so it’s important to make clear that you understand how they are feeling, that it is not their fault, and that you are willing to help.
If you are a young person having these challenges yourself, utilizing coping strategies such as exercise, meditative relaxation, speaking to a trusted adult, and keeping a journal can aid in improving emotional regulation. Also remember that it is a sign of strength, not weakness, to ask for help. You can contact the 988 Suicide & Crisis Lifeline or The Child Center’s main wellness center number at 718-358-8288. Anyone who is actively suicidal should go to the nearest emergency room.
Having good mental health is essential to living a happy and productive life. It affects how we feel, think, and live our lives. A study from the U.S. Department of Health and Human Services found that approximately 60% of those who committed suicide had a mental health diagnosis such as major depression or bipolar disorder. This demonstrates the link between mental health and suicide, as well as how early mental health interventions and self-care can help minimize the number of suicide deaths.
I became a social worker because at its heart, social work is about assisting people when they need it most. Everyone deserves to have a happy and fulfilling life. We should all have someone in our lives who is willing to help us reach our truest self and potential. Our youth are our future, and I am honored to be a part of a profession and organization that is helping solve the mental health crisis.
Editor’s Note, updated September 11, 2023: If you are actively suicidal, go to your nearest emergency room or call 911. For anyone who is experiencing suicidal thoughts, help is available.
- 988 Suicide & Crisis Lifeline: https://988lifeline.org/
- The Child Center of NY wellness centers: 718-358-8288
- Additional resources: https://www.speakingofsuicide.com/resources/